When we think of healthcare design, it is easy to identify some of the more obvious areas of impact in post-pandemic design: patient rooms, circulation, isolation, sanitation, workflow…. Realistically, trends we are seeing today that are being incorporated, either in existing facilities or in tomorrow’s hospitals, are just the beginning. Here, we will explore the trends that Healthcare is currently incorporating into the designs of its facilities:
Spatial Considerations
Markers
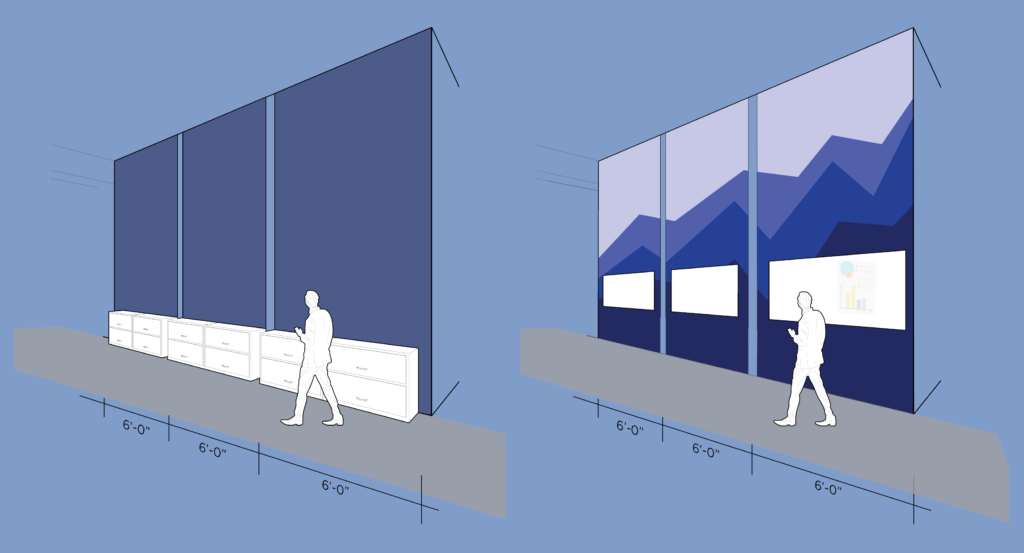
Incorporating the use of material or pattern changes in flooring or wall art strategically reinforces best practices during pandemic times. Utilizing floor markers can help direct circulation flow for patients, staff and physicians. By incorporating these cost-effective changes, providers can indicate one-way aisles, entry and exit ways, and areas where PPE may/may not be required. Wall markers can be applied as a similar concept to floor markers. Using artwork such as murals, vinyl decals or illustrations indicate the appropriate measure and distance between patients, staff and physicians. These visual aids also serve as an aesthetic or artistic feature, as well as provide an opportunity for informational signage. These often can provide a more adaptable means of visualizing six feet of separation.
Furniture and Seating
A waiting room filled with rows of chairs will become a thing of the past. We anticipate providers will begin incorporating more lounge-style seating with adequate space for practicing social distance. We will also see incorporation of more easily cleaned, antimicrobial and naturally sanitizing surfaces in patient areas. While materials like copper may be more cost-prohibitive to some, more cost-effective approaches include hard surfaces, chair coverings that can be wiped down, and incorporating plants that naturally purify the air.
Hallways and Aisles
In addition to markers and seating, consider wider aisles for primary circulation spaces. Hallways and aisleways in hospitals become overflow space for patient care essentials, causing walkways to become cluttered. Patient rooms and hallways that may have not been designed with infectious disease control in mind are especially susceptible to this. Post-COVID, wider aisles may become more common in design to accommodate people passing each other safely while maintaining six feet of distance.
Psychological Considerations
Perceptions of a Safe Environment
Safety for patients, families and staff when interacting with COVID or potential-COVID patients is imperative. What these individuals experience using their five senses impacts their impression of how healthcare providers are addressing pandemic matters. As there are no mandates regulating healthcare providers approach to providing safe environments surrounding COVID, the methodologies we are seeing are different and ever evolving. It is important to note that at this time, healthcare facilities are not consistent in the measures they are taking. Variables such as the spread in their community effect response and protocol. However, measures we are seeing being implemented include temperature monitoring, increased hand sanitizer availability, requiring masks, prohibiting or restricting visitors, among others.
Visual cues
Seek to include visual cues at key moments of risk or transition: for example, doors into patient rooms, PPE storage and access locations, and thresholds between different areas of risk. We will see new construction have more negative pressure rooms and renovations to add them in existing facilities.
Automation
Healthcare providers have always been early adopters of automation technology, and COVID will continue to push additional upgrades to limit exposure and transfer of dangerous germs. While design considerations like automatic doors or digital/keyless/wave entry are commonplace today, we will see more automatic interior doors, or incorporating design of corridors in such a way that doors would not need to be utilized for separation. Hands free technology for sanitizer or hand washing is also well adopted but look forward to robots that sanitize common areas and patient rooms automatically. Additional security measures through automated technology will also become more prevalent.
Building Systems Considerations
Mechanical Design
Pre-COVID, we were already experiencing changes in how our engineering partners were approaching mechanical design issues. Changes in regulatory requirements in terms or ventilation and circulation that were commonplace yesterday will be requiring a much different, and more highly regulated, approach moving forward. We are also seeing a rise in the incorporation of negative pressure rooms in healthcare facilities, as well as the ability to quickly convert existing rooms or whole units into negative pressure environments. Identifying areas in the facilities where there may need to be more negative pressure rooms or rooms that are easily convertible, such as diagnostic and treatment areas, allows us to help plan for this should the need ever arise. While top of mind today, we will continue to give more thought to infection prevention best practices, especially in terms of space planning, throughout healthcare facilities on a global level.
Security
Security is also worth considering in post-COVID design. Limiting access to departments either through touch-less entry or check in helps to limit additional exposure. Temperature checks before returning to desks or additional screening protocol may apply. Utilizing early patient screening prior to arrival for appointments via portals is also becoming increasingly popular. We may also see additional security at facility entrances, along with advancing technology to help protect patients and visitors from risks such as reducing the number of exits throughout the facility. Patient screenings at the door prior to coming inside have become quite common, but we may also see trends like thermal monitoring at entry before being allowed inside.
Patient and Visitor Circulation
Whether inpatient or outpatient, how patients and visitors circulate through healthcare facilities will continue to be redesigned. Wider aisles may become more common for primary circulation spaces to accommodate people passing each other six feet apart safely. In areas where this may not be feasible, one-ways may be instituted using signage and floor markers.
Vertical circulation should also be considered. Assessing occupant loads within elevators, identifying the criteria that will be impacts (ie: loading, peak usage times, wait times) will help in planning for reduced capacity. For example, most commercial elevators are designed to hold 10-12 people, but in today’s post-COVID environment, we are anticipating service to be reduced to 1/3 capacity. The realities include ensuring patients and staff will be able to get to their destination while maintaining adequate physical distancing. Additional new technologies to prevent infection are under development by elevator manufacturers. Encouraging use of stairwells for those capable will help to reduce capacity and wait time concerns. Account for queue lines in lobbies due to increased wait times and plan for social distancing protocol. Incorporation of visual markers, like wall or floor markers, to illustrate safe distances in these spaces will also be helpful.
As there are no specific guidelines in place, we must rely on individual approaches to best practices to provide a safe workplace for employees, patient and physicians. ASHRAE, OSHA, FHA, ADA and more regulatory agencies are continuously revising code requirements that will will impact AHCA. While these changes remain under discussion by many of the agencies, there will need to be a period of time allotted to adopt and implement new practices moving forward.
Cost/Benefit Analysis of Potential Changes
 While today our focus is centered around ways we can reduce risk, some of the trends we are seeing can be costly in terms of longevity and return on investment. Some trends may be here to stay, while others will fade with some return to normalcy in terms of best design practices. Healthcare providers will have to determine level of risk that they, their staff and patients are willing to accept as they look at the cost/benefit of the different options.
While today our focus is centered around ways we can reduce risk, some of the trends we are seeing can be costly in terms of longevity and return on investment. Some trends may be here to stay, while others will fade with some return to normalcy in terms of best design practices. Healthcare providers will have to determine level of risk that they, their staff and patients are willing to accept as they look at the cost/benefit of the different options.
Some of the most cost-effective design trends we are recommending to our clients:
Distance: create space for six feet (or 36sf) per person
Equipment: provide PPE for employees who may need it
Cues: add visual cues throughout the spaces to promote best practices
Circulation: create one-ways aisles and wider aisle space for separation
Hygiene: increase sanitation of workstations and frequently touched items
Technology: use technology to supplement your defenses. what types of technology have you already incorporated in your workplace? What methods can you continue to explore?