As we continue to dive into healthcare design in a post-COVID world, the trends we are seeing today and are being incorporated, either in existing facilities or in tomorrow’s hospitals, are just the beginning.
Areas of Social Distance
Safe environments must be provided for patients, family, or staff when they are interacting with COVID or potential COVID patients. Incorporating the six feet of separation between staff and patients is crucial to not only helping stop the spread of harmful germs, but also in providing visible cues that alter psychological responses to how the facility is incorporating best practices.
Waiting Rooms, Registration and Checkout
Registration and checkout areas will be outfitted with plexi screens or other types of barriers to help encourage separation between the various staff and patients. We will also see a greater utilization of technology to aid in standard check in procedures, either touch free (verbal commands) or filling out forms and insurance changes via your phone upon arrival, or even prior to, a patient’s visit. The use of telehealth will expand. Checkout may be performed virtually in the room prior to a patient exiting or by phone to help eliminate additional touchpoints.
Nursing Units and Clinical Areas
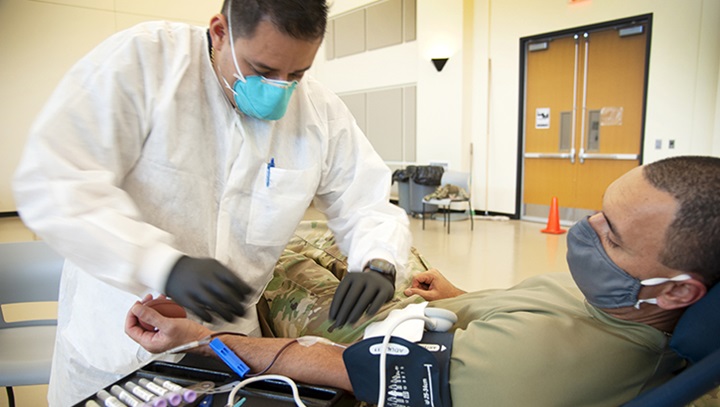
Entire nursing units and ICU units will be designed for patients with respiratory illness (i.e. COVID 19) with dedicated healthcare personnel assigned to these units to limit exposure. These will be negative pressure rooms. Appropriate locations for easily accessible PPE must be provided. New ICU units will be built with the ability to be used as step down units when not in use as ICUs.
Clinical areas where COVID patients are undergoing aerosol generating procedures must also be negative pressure on separate air handling system (i.e., bronchoscopy, nebulizer treatment, sputum induction, BIPAP, CPAP, etc.).
In the Emergency Department, there will be dedicated space for respiratory/COVID-19 patients on a separate air handling system and with the ability to dedicate an area to an ICU level of care to prevent movement of these patients through the facility. The use of outside screening tents prior to coming into the ER will reduce the risk of COVID being spread.
Practicing safe social distancing practices is not new in healthcare. However, we will continue to see the incorporation and adoption of new, safer practices as we continue to learn more and adapt to the repercussions seen as a result of the novel Coronavirus.
Offices and Support areas
We are going to see best practices carry over from today’s workspace into our healthcare office and support areas, and vice versa. In closed office spaces primarily seen in doctor’s offices, much will remain the same. Limited seating and additional distancing from guests may be incorporated, as well as more frequent sanitizing. Spacing of time between appointments will also assist in achieving this.
Open office areas common in the administrative areas of healthcare facilities can expect changes in space between desks and seating areas. PPE (personal protective equipment) may be required in these areas as opposed to just patient rooms as we may be used to experiencing. Additional barriers utilizing materials such as plexiglass may be installed above or surrounding desk areas to limit contact between employees.
Security among departments is also something worth considering. Limiting access to departments either through touchless entry or check in helps to limit additional exposure. Temperature checks before returning to desks or additional screening protocol may apply.
Ancillary Spaces
Places like the cafeterias will also need to be considered. Creating space for social distance throughout the seating areas will limit capacity. Buffets will be eliminated, and that space will be used for additional circulation within the space. Considering additional protective measures, like plexiglass at cashier stations or more prepackaged grab-and-go items, can help to limit contact. Prep areas for meals being delivered to patients’ rooms will also need to be redesigned as will ventilation systems in the food prep areas.
OR Suites
If possible, you may see increased use of laminar flow units in the OR as well as the use of UV technology for additional reduction of risk of infections in the ORs at night after cleaning and sanitizing. Spacing of cases and longer times for turnover will also be practices put into place to prevent spread of infection.

Frequent sanitation of surfaces and equipment will be necessary.
Outpatient Facilities
Even prior to COVID-19, we were seeing more focus on outpatient facilities. Ambulatory surgery centers, freestanding ERs, urgent care, physician offices and freestanding labs are becoming more and more common as reliable, safe healthcare options in lieu of hospitals. More procedures are being moved out of the hospital safely into the outpatient setting.
The design of these spaces must keep staff, physicians and patients safe. In addition to the considerations above, seek to include visual cues at key moments of risk or transition: for example, doors into patient rooms, PPE storage and access locations, and thresholds between different areas of risk. We will see new construction have more negative pressure rooms and renovations to add them in existing facilities.
Warehouse Space
Thinking beyond the walls of the healthcare facility, the development and delivery of medical devices and equipment will also face new challenges in design. New requirements for PPE and other medical supplies, instead of a JIT system that is commonly found in pre-COVID design, will require us to think through spatial considerations in terms of storage.
It should also be noted that as the manufacturing industry continues to increase, so does the production for medical equipment that has been depleted due to reactive measures. Access to affordable protective equipment, through additional logistics, manufacturing and transportation methods, will continue to increase.
Health care systems may lease or build large warehouses centrally located to the hospitals in their system to accommodate this necessary storage.
Patient and Visitor Circulation
Whether inpatient or outpatient, how patients and visitors circulate through healthcare facilities will continue to innovate as best practices are adopted. Wider aisles may become more common for primary circulation spaces to accommodate people passing each other six feet apart safely. In areas where this may not be feasible, one-ways may be instituted using signage and floor markers. The incorporation of fewer or one-way entry and exit into different areas or wings will become more common. Restricted access may be instituted and managed using automated technology or even facial recognition. Areas where risk of transmission is greater, such as patient rooms, will see additional barriers in place, more accessibility to proper sanitation, as well as use of appropriate PPE when entering patient rooms. Consider best practices for removal and disposal of PPE upon exiting.

Social distancing markers in elevators.





